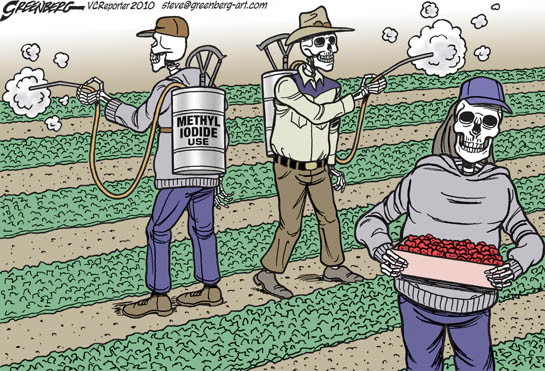
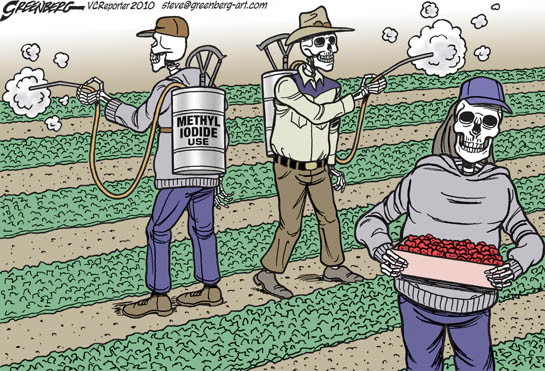
Pesticides are anything applied to control or eliminate a pest. Pests can be anything from insects to weeds to fungus.
Pesticides like weed control, weed and feed, and pre-emergents can cause short-term adverse health effects, called acute effects, as well as chronic adverse effects that can occur months or years after exposure. Examples of acute health effects include stinging eyes, rashes, blisters, blindness, nausea, dizziness, diarrhea and death. Examples of known chronic effects are cancers, birth defects, reproductive harm, immunotoxicity, neurological and developmental toxicity, and disruption of the endocrine system.
Some people are more vulnerable than others to pesticide impacts. For example, infants and young children are known to be more susceptible than adults to the toxic effects of pesticides. Farm workers and pesticide applicators are also more vulnerable because they receive greater exposures.
For more information about the effects of specific chemicals or pesticide products, see Pesticide Action Network’s Pesticide Database. For a survey of scientific studies linking pesticides to specific diseases, see Beyond Pesticides’ Pesticide-induced diseases database.
Acute (Immediate) Health Effects
Immediate health effects from pesticide exposure includes irritation of the nose, throat, and skin causing burning, stinging and itching as well as rashes and blisters. Nausea, dizziness and diarrhea are also common. People with asthma may have very severe reactions to some pesticides, particularly pyrethrin/pyrethroid, organophosphate and carbamate pesticides.
In many cases, symptoms of pesticide poisoning mimic symptoms of colds or the flu. Since pesticide-related illnesses appear similar or identical to other illnesses, pesticide poisonings are often misdiagnosed and under-reported. Immediate symptoms may not be severe enough to prompt an individual to seek medical attention, or a doctor might not even think to ask about pesticide exposure. Still, seek medical attention immediately if you think you may have been poisoned by pesticides.
Chronic (Long-term) Health Effects
Chronic health effects include cancer and other tumors; brain and nervous system damage; birth defects; infertility and other reproductive problems; and damage to the liver, kidneys, lungs and other body organs. Chronic effects may not appear for weeks, months or even years after exposure, making it difficult to link health impacts to pesticides.
Pesticides have been implicated in human studies of leukemia, lymphoma and cancers of the brain, breasts, prostate, testes and ovaries. Reproductive harm from pesticides includes birth defects, still birth, spontaneous abortion, sterility and infertility.
Endocrine disruptors are chemicals that — often at extremely low doses — interfere with important bodily functions by mimicking or blocking hormones (the chemical messengers that circulate in blood and regulate many body processes including metabolism, brain development, the sleep cycle and stress response). Some pesticides act as endocrine disruptors and have been shown to cause serious harm to animals, including cancer, sterility and developmental problems. Similar impacts have been associated with human exposure to these chemicals.
Children are More Vulnerable to Pesticide Exposure
Children are not simply “little adults.” Children are more vulnerable to pesticide exposure because their organs, nervous systems and immune systems are still developing. Children are also less able to detoxify and excrete pesticides. Exposure during certain early development periods can cause permanent damage.
In addition to being more vulnerable to pesticide toxicity, children’s behavior and physiology make them more likely to receive greater pesticide exposure than adults. Most pesticide exposure occurs through the skin and children have more skin surface for their size than adults. Children have a higher respiratory rate and so inhale airborne pesticides at a faster rate than adults. Children also consume proportionately more food and water — and pesticide residues — than adults. With their increased contact with floors, lawns and playgrounds, children’s behavior also increases their exposure to pesticides.
Health Effects of Certain Classes of Pesticides
Organophosphates & Carbamates: These pesticides are like nerve gas: they attack the brain and nervous system, interfering with nerve signal transmission. Symptoms include headaches, nausea, dizziness, vomiting, chest pain, diarrhea, muscle pain and confusion. In severe poisoning incidents, symptoms can include convulsions, difficulty breathing, involuntary urination, coma and death. Acute poisoning of the nervous system by these pesticides affects hundreds of thousands of people around the world each year.
Soil Fumigants: These pesticides are applied to soil, forming a gas that is toxic to nematodes, fungi, bacteria, insects, and plants in the soil. Because they are gases, they move from the soil into the air and expose people living or working nearby. Commonly used soil fumigants in California include 1,3-dichloropropene, chlorpicrin, metam sodium, and metam potassium. Symptoms of fumigant exposure include irritation of skin, eyes, and lungs (dichloropropene and chloropicrin), and extremely irritating to eyes and lungs (metam sodium and metam potassium). Dichloropropene, metam sodium, and metam potassium are all cancer causing chemicals and metam sodium causes reproductive harm. In counties where fumigant use is high, premature birth is more common than in counties with low fumigant use.
Pyrethroids: These insecticides are synthetic chemicals that are structurally similar to botanical compounds but have been designed to be more persistent. They are toxic to the nervous system, and there is concern that during pregnancy a fetus is not able to efficiently break down these chemicals. Symptoms of pyrethroid poisoning include tremors, salivation, headache, fatigue, vomiting, stinging and itching skin, and involuntary twitching.
Many pyrethroids also cause long term health problems. For example, resmethrin causes both cancer and reproductive harm. Cypermethrin, fenvalerate, and deltamethrin all cause genetic damage and reproductive harm. Data from the Center for Disease Control and Prevention’s national biomonitoring program links pyrethroid exposure to heart disease.
Source:
https://www.pesticidereform.org/pesticides-human-health/
Hazards of Chemical Lawn Care to Humans
Studies show that hazardous lawn chemicals are drifting into our homes where they contaminate indoor air and surfaces, exposing children to levels ten times higher than pre-application levels. Of 40 most commonly used lawn pesticides, 26 are linked with cancer or carcinogenicity, 12 are linked with birth defects, 21 with reproductive effects, 32 with liver or kidney damage, 24 with neurotoxicity, and 24 with disruption of the endocrine (hormonal) system.
 Of those same 40 lawn pesticides, 21 are detected in groundwater, 24 have the ability to leach into drinking water sources, 39 are toxic to fish and other aquatic organisms vital to our ecosystem, 33 are toxic to bees, 18 are toxic to mammals, and 28 are toxic to birds. With numbers like this, the only logical question becomes: is this really necessary and what can we do to stop or prevent this kind of contamination?
Of those same 40 lawn pesticides, 21 are detected in groundwater, 24 have the ability to leach into drinking water sources, 39 are toxic to fish and other aquatic organisms vital to our ecosystem, 33 are toxic to bees, 18 are toxic to mammals, and 28 are toxic to birds. With numbers like this, the only logical question becomes: is this really necessary and what can we do to stop or prevent this kind of contamination?
Members of the National Coalition for Pesticide-Free Lawns are working to halt senseless exposure to lawn pesticides and to educate the public, landscapers, and policy makers on the use of non-toxic and least-toxic lawn care practices and products. Change begins at local level. The public plays an extremely important role in lawn pesticide reform – not only in the way it perceives the use of toxic pesticides in homes and communities but also in the way it demands safe alternatives from retailers, organic services from lawn care providers, and better protection from pesticide exposure from local policy makers.
Source:
https://www.beyondpesticides.org/resources/lawns-and-landscapes/overview/hazards-and-alternatives
Yard chemicals can be absorbed through skin & inhaled.
The Facts about lawn chemicals, what can you do?
When using lawn chemicals, become familiar with a product’s toxicity and potential environmental impact.
The following are some of the health risks that lawn chemicals pose to humans, pets, wildlife and aquatic organisms.
The use of lawn chemicals accounts for the majority of wildlife poisonings reported to the Environmental Protection Agency.
Lawn chemicals can be absorbed through the skin, swallowed or inhaled.
During application, lawn chemicals can drift and settle on ponds, laundry, toys, pools and furniture.
Even pets are at risk — studies show that the rates of lymphoma in pets of pesticide users are significantly higher than occurrences in the pets of non-chemical users. Several types of cancer, immuno-response deficiencies, neurological diseases, and birth defects have been associated with exposure to lawn chemicals. By releasing chemical toxins into the environment, air and water quality suffer, ultimately causing health problems.
Lawn chemicals are the fertilizers, herbicides and insecticides used in lawn and garden care. When lawn chemicals are applied improperly, they can run off into streams, harming fish and other animals and contaminating our drinking water. Overapplication of any lawn chemical can result in runoff that carries toxic levels of chemicals or excessive nutrients into lakes, streams and groundwater. Fertilizers usually contain nitrogen, phosphorous and potassium (potash). Nitrogen is an important lawn nutrient, but it can contaminate groundwater with nitrates. Phosphorous can promote excess weed growth in lakes and ponds and contaminate groundwater, while the chloride that is often combined with potassium in potash is also harmful.
Some lawn chemicals threaten native flowers and grasses by harming beneficial insects that safely control weeds and unwanted insects. What’s the Problem?
When lawn chemicals run off into lakes and streams, off into lakes and streams, off into lakes and streams, insects and fish are harmed or killed, causing disruption to the entire food chain.
Fortunately, there are some things that you can do to lessen the effect lawn chemicals have on water quality: Read labels on lawn chemicals carefully and always apply products sparingly. Try using compost or organic lawn chemical alternatives. Composting creates an organic, slow-release fertilizer and soilenhancing material. Landscape with native plants, grasses and flower species whenever possible.
A natural lawn reduces or eliminates the need for lawn chemicals. Use caution on slopes and lawn edges so fertilizer will not wash into nearby storm sewers or waterways. Allow proper drying time for liquid chemicals, and never use lawn chemicals before a heavy rainfall is expected. Test the soil for nutrient deficiencies before using lawn chemicals. Contact your county extension service for more information on lawn chemical use.
Extension phone numbers can be found at www.marc.org/water. The improper use of lawn chemicals threatens the quality of our water What is a Watershed? A watershed is an area of land that drains to a common point, such as a nearby creek, stream, river or lake. Every small watershed drains to a larger watershed that eventually flows to the ocean. Watersheds support a wide variety of plants and wildlife and provide many outdoor recreation opportunities. By protecting the health of our watersheds we can preserve and enhance the quality of life for Kansas City area residents.
For more information, visit www.marc.org/water .marc.org/water or call 816/474-4240. or call 816/474-4240.
Good Neighbors Care About Clean Water
Source:
https://cfpub.epa.gov/npstbx/files/marc_lawnchemicals.pdf
Dangers of Chemical Lawn Pesticides & Fertilizers
https://www.rd.com/article/lawn-fertilizer-dangers/
The Dark Side of the Perfectly Manicured American Lawn: Is It Giving You Cancer?
From the book Contamination
Your grass may be greener than your neighbor's, but at what price?
 YASU+JUNKO FOR READER'S DIGEST
YASU+JUNKO FOR READER'S DIGEST
On a beautiful April day, I decided to meet outside with my students at the University of Delaware, where I teach journalism. We sat on the central lawn between two buildings that just happened to bear the names of two gargantuan chemical companies: DuPont and Gore. In the middle of a conversation about agricultural pesticides, a groundskeeper, dressed from feet to neck in a white chemical suit, drove by us on a mower. He wasn’t cutting the grass, though; he was spraying it. And not from one nozzle, but from half a dozen. Up and back he went, describing parallel lines as neat as those in any Iowa farmer’s cornfield. Not a blade escaped the spray. This became a perfect teaching moment.
“Who’s going to ask him what he’s spraying?” I asked my students. One young woman marched over to the groundskeeper. He turned off his engine, they spoke, and she returned.
“He said he’s spraying 2,4-D,” she said. “He said we didn’t need to worry, because he sprayed where we’re sitting at five this morning.”
Which would mean about seven hours earlier. My students chuckled uneasily. He was wearing a full-body chem suit, and they were sitting on the grass in shorts and bare feet?
They’d never heard of 2,4-D, or 2,4-dichlorophenoxyacetic acid. But they had heard of Agent Orange, the notorious defoliant used in Vietnam, and 2,4-D, one of the most extensively used herbicides in the world, is a constituent of Agent Orange (it did not cause the bulk of the devastating effects associated with Agent Orange). It was developed during World War II, mostly as a weapon to destroy an enemy’s rice crops. Despite its history, 2,4-D has long been seen as safe for consumer use.
In the 1940s, botanist E. J. Kraus of the University of Chicago fed five and a half grams of pure 2,4-D to a cow every day for three months. The cow was fine, according to Kraus, as was her calf. Kraus said he himself had eaten half a gram of the stuff every day for three weeks and felt great. This was apparently good enough for the rest of the country; within five years, American companies were annually producing 14 million pounds of the stuff. By 1964, the number had jumped to 53 million pounds.
Today, annual sales of 2,4-D have surpassed $300 million worldwide, and it’s found in “weed and feed” products, like Scotts Green Sweep, Ortho Weed B Gon, Salvo, Weedone, and Spectracide. At first, its impact on humans seems mild—skin and eye irritation, nausea, vomiting, dizziness, stiffness in the arms and legs—and many lawn-care companies have dismissed health concerns. Plus, the businesses add that the amount of chemicals in sprays is very diluted.
[pullquote] With 80 million home lawns and over 16,000 golf courses, you get close to 50 million acres of cultivated turf in America. [/pullquote]
But the effects are more worrisome when considered over time. Because 2,4-D is designed to mimic a plant’s natural growth hormone, it causes such rapid cell growth that the stems of treated plants tend to become grotesquely twisted and their roots swollen; the leaves turn yellow and die; and the plants starve to death (2,4-D does not have this effect on grass).
Unsurprisingly, 2,4-D also appears to affect human hormones. The National Institute of Health Sciences lists it as a suspected endocrine disrupter, and several studies point to its possible contribution to reproductive-health problems and genetic mutations. Although the EPA says there isn’t enough evidence to classify 2,4-D as a carcinogen, a growing body of research has begun to link it to a variety of cancers.
A 1986 National Cancer Institute (NCI) study found that farmers exposed to 2,4-D for 20 or more days a year had a sixfold higher risk of developing non-Hodgkin’s lymphoma. Another NCI study showed that dogs were twice as likely to contract lymphoma if their owners used 2,4-D on their lawns.
Like flame retardants, this compound also tends to accumulate inside people’s homes even days after the lawn has been sprayed. One study found 2,4-D in the indoor dust of 63 percent of sampled homes; another showed that levels of the chemical in indoor air and on indoor surfaces increased after lawn applications. After 2,4-D was sprayed, exposure levels for children were ten times higher than before the lawns were treated—an indication of how easily the chemical is tracked inside on the little feet of dogs, cats, and kids.
Thanks to pressure from campus activists, my university replaced 2,4-D with “softer” herbicides and began putting signs on lawns that had just been sprayed. Of course, 2,4-D is one of scores of pesticides in use. According to David Pimentel, professor emeritus of entomology at Cornell University, 110,000 people suffer adverse health effects from pesticides every year, and 10,000 cases of cancer in humans may be attributable to pesticide exposure.
The Greening of America
In 1900, 60 percent of Americans lived in rural areas. Today, 83 percent live in cities or suburbs. With that change has come an astonishing shift in the landscape. Over the past half century, Americans have become obsessed with grass. When you add up the country’s 80 million home lawns and over 16,000 golf courses, you get close to 50 million acres of cultivated turf in the United States, an expanse roughly the size of Nebraska. This space is growing by 600 square miles a year.
By 1999, more than two thirds of America’s home lawns had been treated with chemical fertilizers or pesticides—14 million by professional lawn-care companies. A year later, the U.S. General Accounting Office reported that Americans were spraying 67 million pounds of synthetic chemicals on their grass every year, and annual sales of lawn-care pesticides had grown to $700 million.
The landscaping trucks rolling through our suburban neighborhoods seem to represent something more than a communal desire for lush grass. Could it be relief from anxiety? (Why else call a company Lawn Doctor?) For one thing, hiring lawn-care specialists is a public declaration that you have the money not to take care of your yard yourself.
Diligent lawn maintenance and chemical use are also associated with approval and social status, Ohio State researchers reported in 2012: “The main factor influencing a homeowner’s decision to use lawn chemicals is whether neighbors or other people in the neighborhood use them. Homeowners crave acceptance from their neighbors and generally want their lawns to fit in with their surrounding community, so they adopt their neighbors’ practices.”
We also create manicured lawns to play the most chemically dependent of pastimes: golf. By 2004, there were just under 15,000 golf courses in the United States—a patchwork of chemically treated turf the size of Rhode Island and Delaware combined.
Even grass seed comes coated with chemicals. A close look at a bag of Scotts grass seed reveals it has been treated with Apron XL fungicide, whose active ingredient is Metalaxyl-M, or methyl N-(methoxyacetyl)-N-(2,6-xylyl)-D-alaninate. The bag requests that the product be stored away from foodstuffs, kept out of the reach of children, and not be applied near water, storm drains, or drainage ditches. (A Scotts spokesperson says that its products are designed to be safe when used as directed.)
As the use of chemicals has become widespread, lawn companies have found an unexpected source of profits. Herbicides like 2,4-D preserve grass but kill weeds like clover. Clover, however, pulls nitrogen out of the air and fixes it in the soil. Without clover, soil becomes nitrogen poor and fails to support plant life. So chemical companies now replace the depleted nitrogen, which homeowners used to get for free from clover, with synthetic nitrogen, for which they have to pay.
In America’s watersheds, nitrogen runoff is considered among the worst problems for water quality. Since synthetic fertilizers are water soluble, a good amount runs off your lawn after a rain, where it mixes with runoff from other homes and ends up feeding the plants in bodies of water. Doused with chemicals, algae grow and grow, creating “algae blooms” that—as they decay and die—suck most of the oxygen out of rivers, lakes, and bays and lead to massive “dead zones,” in which neither fish nor plants can live.
In 2007, the Chesapeake Bay Foundation published a report card on the bay’s health that showed just how much trouble chemicals can pose. The bay received an F for nitrogen pollution, a D-minus for phosphorous, an F for water quality, an F for dissolved oxygen, and a D for toxics. On a scale of 100 (with 100 being the best), the bay’s health was rated at 28.
In California, scientists are discovering that algae blooms off the coast not only remove oxygen; they also release a toxin, domoic acid. It enters the food chain when fish eat algae, then moves into the sea lions that consume the fish. If a sea lion is pregnant, her fetus can be contaminated, and years later, that mammal may develop epilepsy.
Kids and Pesticides Don't Mix
Note: Pesticides refer to weed killers, fungicides, insecticides, and animal repellents.
Children are especially vulnerable to pesticides The National Academy of Sciences reports that children are more susceptible to chemicals than adults and estimates that 50% of lifetime pesticide exposure occurs during the first five years of life.1 EPA concurs that children take in more pesticides relative to body weight than adults and have developing organ systems that are more vulnerable and less able to detoxify toxic chemicals.2 Infants crawling behavior and proximity to the floor account for a greater potential than adults for dermal and inhalation exposure to contaminants on carpets, floors, lawns, and soil.3 Children with developmental delays and those younger than six years are at increased risk of ingesting pesticides through nonfood items, such as soil.4 Pre-natal exposure to the herbicide atrazine are associated with fetal growth restriction and small head circumference and fetal growth restriction.5 A 2010 analysis observed that women who use pesticides in their homes or yards were two times more likely to have children with neural tube defects than women without these reported exposures.6 Studies find that pesticides such as the weedkiller 2,4-D pass from mother to child through umbilical cord blood and breast milk.7 Consistent observations have led investigators to conclude that chronic low-dose exposure to certain pesticides might pose a hazard to the health and development of children.8 The World Health Organization (WHO) cites that over 30% of the global burden of disease in children can be attributed to environmental factors, including pesticides.9 Children, cancer and pesticides In 2015, WHO found that there was sufficient evidence of carcinogenicity in experimental organisms to classify glyphosate, the active ingredient in the most popular lawncare brand (Roundup) as “probably carcinogenic to humans” (Group 2A). WHO also found that 2,4-D- found in many ‘weed and feed’ products- is possibly carcinogenic.10 A 2010 meta-analysis of 15 studies on residential pesticide use and childhood leukemia finds an association with exposure during pregnancy, as well as to insecticides and herbicides. An association is also found for exposure to insecticides during childhood. 11 A 2013 study suggests that preconception pesticide exposure, and possibly exposure during pregnancy, is associated with an increased risk of childhood brain tumors.12 According to a 2015 study, living in agricultural regions is linked to increased leukemia and central nervous system cancers in children.13 A meta-analysis study by scientists at the Harvard University’s School of Public Health finds that children’s exposure to pesticides in and around the home results in an increased risk of developing certain childhood cancers. Authors found that cancer risks were connected most closely to the type of pesticide used and the location where it was applied.14 The probability of an effect such as cancer, which requires a period of time to develop after exposure, is enhanced if exposure occurs early in life.15 A study published in the Journal of the National Cancer Institute finds that household and garden pesticide use can in- Don’t Mix A Beyond Pesticides Fact Sheet n A Beyond Pesticides Fact Sheet n A Beyond Pesticides Fact Sheet Children and Pesticides Commonly Used Chemicals Chemical Common Use Health Effects 2,4-D Lawns c, ed, r, n, kl, si, bd Dicamba Lawns r, n, kl, si, bd Fipronil Indoor/outdoor c, ed, n, kl, si baits, pet care Glyphosate Lawns c, r, n, kl, si Permethrin Mosquitoes, c, ed, r, n, kl, si head lice, garden Key: Birth/developmental defects=bd; Kidney/liver damage=kl; Sensitizer/irritant=si; Cancer=c; Neurotoxicity=n; Endocrine Disruption=ed; Reproductive effects=r Alternatives Reduce exposure to toxic chemicals by adopting sound organic or integrated pest management (IPM) practices that use cultural, mechanical and biological methods of control and least-toxic chemicals only as a last resort. An organic diet limits children’s pesticide exposure and toxic body burden. crease the risk of childhood leukemia as much as seven-fold.16 Studies show that children living in households where pesticides are used suffer elevated rates of leukemia, brain cancer and soft tissue sarcoma.17 Pesticides can increase susceptibility to certain cancers by breaking down the immune system’s surveillance against cancer cells. Infants and children, the aged and the chronically ill are at greatest risk from chemically-induced immune suppression.18 A study published by the American Cancer Society finds an increased risk for non-Hodgkin’s lymphoma (NHL) in people exposed to common herbicides and fungicides, particularly the weedkiller mecoprop (MCPP). People exposed to glyphosate (Roundup®) are 2.7 times more likely to develop NHL.19 75 out of all 99 human studies done on lymphoma and pesticides find a link between the two.20 Four peer-reviewed studies demonstrate the ability of glyphosate-containing herbicides to cause genetic damage to DNA (mutagenicity), even at very low concentration levels.21 A 2007 study published in Environmental Health Perspectives finds that children born to mothers living in households with pesticide use during pregnancy had over twice as much risk of getting cancer, specifically acute leukemia (AL) or nonHodgkin lymphoma (NHL).22 A 2007 Canadian report shows that a greater environmental risk exists for boys, specifically when it comes to cancer, asthma, learning and behavioral disorders, birth defects and testicular dysgenesis syndrome.23 Children, asthma and pesticides Researchers find that pesticides may increase the risk of developing asthma, exacerbate a previous asthmatic condition or even trigger asthma attacks by increasing bronchial hyper-responsiveness. 24 Studies show children’s developing organs create “early windows of great vulnerability” during which exposure to pesticides can cause great damage. One 2015 farmworker study found an association between early-life exposure to OPs and respiratory symptoms consistent with possible asthma in childhood.25 A 2012 study concluded that prenatal PBO exposure was associated with childhood cough in inner city children.26 A 2004 study finds that young infants and toddlers exposed to herbicides (weedkillers) within their first year of life are 4.5 times more likely to develop asthma by the age of five, and almost 2.5 times more likely when exposed to insecticides.27 EPA material safety data sheets for the common herbicides 2,4-D, mecoprop, dicamba, (often combined as Trimec®) and glyphosate (Roundup®) list them as respiratory irritants that can cause irritation to skin and mucous membranes, chest burning, coughing, nausea and vomiting. Children, learning and developmental disorders and pesticides Roughly one in six children in the U.S. has one or more developmental disability, ranging from a learning disability to a serious behavioral or emotional disorder.28 Scientists believe that the amount of toxic chemicals in the environment that cause developmental and neurological damage are contributing to the rise of physical and mental effects being found in children.29 According to researchers at the University of CaliforniaBerkeley School of Public Health, exposure to pesticides while in the womb may increase the odds that a child will have attention deficit hyperactivity disorder (ADHD).30 Studies show children’s developing organs create “early windows of great vulnerability” during which exposure to pesticides can cause great damage.31 Lawn pesticide products containing herbicides and fertilizers A Beyond Pesticides Fact Sheet n A Beyond Pesticides Fact Sheet n A Beyond Pesticides Fact Sheet A Beyond Pesticides Fact Sheet n A Beyond Pesticides Fact Sheet n A Beyond Pesticides Fact Sheet (such as “weed and feed” products) tested on mice show increased risk of infertility, miscarriage and birth defects at very low dosages.32 Results from a CHARGE study finds that agricultural exposures to organophosphates at some point during gestation was associated with a 60% increased risk for austism higher for third-trimester exposures, and second-trimester chlorpyrifos applications. Similarly, children of mothers residing near pyrethroid insecticide applications just before conception or during third trimester were at greater risk for both autism and developmental delay.33 Researchers at the Cincinnati Children’s Hospital Medical Center found an association between increasing pyrethroid pesticide exposure and ADHD which they conclude may be stronger for symptoms seen in boys compared to girls.34 Additional studies on lawn pesticide product formulations show effects on learning ability, aggressiveness, memory, motor skills and immune system function.35 A 2002 study finds children born to parents exposed to glyphosate (Roundup®) show a higher incidence of attention deficit disorder and hyperactivity.36 A study of 210,723 live births in Minnesota farming communities finds children of pesticide applicators have significantly higher rates of birth defects than the average population.37 In a 2004-2005 review of 2,4-D, EPA finds that, “there is a concern for endocrine disruption.”38 Pesticide accumulation and drift Children ages 6-11 nationwide have significantly higher levels of pesticide residues in their bodies than all other age categories.39 Biomonitoring testing in Canada finds residues of lawn pesticides, such as 2,4-D and mecoprop, in 15 percent of children tested, ages three to seven, whose parents had recently applied the lawn chemicals. Breakdown products of organophosphate insecticides are present in 98.7 percent of children tested.40 Scientific studies show that 2,4-D applied to lawns drifts and is tracked indoors where it settles in dust, air and surfaces and may remain for up to a year in carpets.41 One 2014 analysis of 129 preschool children, ages 20 to 66 months, found that children were exposed to indoor concentrations of pyrethroids, organophosphates and organochlorines pesticides which were detected in soil, dust and indoor air.42 Samples from 120 Cape Cod homes, where elevated incidence of breast, colorectal, lung, and prostate cancers are reported, find high indoor air and dust concentrations of carbaryl, permethrin, and 2,4-D.43 A study published in Environmental Health Perspetives found that children who eat a conventional diet of food produced with chemical-intensive practices carry residues of organophosate pesticides that are reduced or eliminat- ed when they switch to an organic diet.44 Scientists at the California Department of Public Health found that 28% of the mothers studied who lived near fields in the Central Valley, which were sprayed with organo- chlorines, such as endosulfan and dicofol, have children with autism.45 A 2005 study published in the Journal of the American Medical Association found that students and school em- ployees are being poisoned by pesticide use at schools and from drift off of neighboring farmlands.46 Endnotes 1. National Research Council, National Academy of Sciences. 1993. Pesticides in the Diets of Infants and Children, National Academy Press, Washington, DC. 184-185. 2. US EPA, Office of the Administrator, Environmental Health Threats to Children, EPA 175-F-96-001, September 1996. See also: http://www.epa.gov/pesticides/ food/pest.htm. 3. Bearer, CF. 2000. “The special and unique vulnerability of children to environmental hazards.” Neurotoxicology 21: 925-934; Fenske, R., et al. 1990. “Potential Exposure and Health Risks of Infants following Indoor Residential Pesticide Applications.” Am J. Public Health. 80:689-693. 4. Faustman EM, Silbernagel SM, Fenske RA, Burbacher TM, Ponce RA. 2000. “Mechanisms underlying children’s susceptibility to environmental toxicants.” Environmental Health Perspectives. 108(suppl 1):13 –21. 5. Chevrier C, Limon G, Monfort C, Rouget F, Garlantézec R, Petit C, et al. 2011. Urinary Biomarkers of Prenatal Atrazine Exposure and Adverse Birth Outcomes in the PELAGIE Birth Cohort. Environ Health Perspect. 119:1034-1041 6. Brender, JD., et al. 2010. Maternal Pesticide Exposure and Neural Tube Defects in Mexican Americans. Ann Epidemiol. 20(1):16-22 7. Pohl, HR., et al. 2000. “Breast-feeding exposure of infants to selected pesticides,” Toxicol Ind Health 16 :65 –77; Sturtz, N., et al. 2000. “Detection of 2,4-dichlorophenoxyacetic acid (2,4-D) residues in neonates breast-fed by 2,4-D exposed dams.” Neurotoxicology 21(1-2): 147-54; Houlihan, J., et al. 2005. Body Burden, The Pollution in Newborns. Environmental Working Group, Washington, D.C. http://www.ewg.org/reports/body_burden2/ (accessed8/5/05). 8. Weiss, B., et al. 2004 April. “Pesticides,” Pediatrics 113(4): 1030-1036. 9. World Heath Organization (WHO). 2006. Principles for Evaluating Health Risks in Children Associated with Exposure to Chemicals. Geneva, Switzerland. 10. [IARC. IARC Monographs Volume 112: evaluation of five organophosphate insecticides and herbicides. 20 march 2015. http://www.iarc.fr/en/media-centre/iarcnews/pdf/MonographVolume112.pdf; and IARC. Carcinogenicity of lindane, DDT, and 2,4-dichlorophenoxyacetic acid. The Lancet Oncology, 16(8).p891-892. 11. Turner, M.C., et al. 2010. Residential pesticides and childhood leukemia: a systematic review and meta-analysis. Environ Health Perspect 118(1):33-41
12. Green KR, Peters S, Bailey HD. 2013) Exposure to pesticides and the risk of childhood brain tumors. Cancer Causes Control. DOI 10.1007/s10552-013-0205-1 13. Booth BJ, Ward MH, Turyk ME, et al. 2015. Agricultural crop density and risk of childhood cancer in the midwestern United States: an ecologic study. Environmental Health:14(82) 14. Chen M, Chi-Hsuan C, Tao L, et al. 2015. Residential Exposure to Pesticide During Childhood and Childhood Cancers: A Meta-Analysis. Pediatrics. DOI: 10.1542/ peds.2015-0006 15. Vasselinovitch, S., et al. 1979. “Neoplastic Response of Mouse Tissues During Perinatal Age Periods and Its Significance in Chemical Carcinogensis,” Perinatal Carcinogenesis, National Cancer Institute Monograph 51. 16. Lowengart, R., et al. 1987. “Childhood Leukemia and Parent’s Occupational and Home Exposures,” Journal of the National Cancer Institute 79:39. 17. Leiss, J., et al. 1995. “Home Pesticide Use and Childhood Cancer: A Case-Control Study,” American Journal of Public Health 85:249-252; Gold, E. et al. 1979. “Risk Factors for Brain Tumors in Children,” Am J of Epidemiology 109(3): 309-319; Lowengart, P., et al. 1995. “Childhood Leukemia and Parents’ Occupational and Home Exposures,” J National Cancer Institute 79(1): 39-45; Reeves, J. 1982. “Household Insecticide-Associated Blood Dyscrasias in Children,” (letter) Am J of Pediatric Hematology/Oncology 4:438-439; Davis, J., et al. 1993. “Family Pesticide Use and Childhood Brain Cancer,” Archives of Environmental Contamination and Toxicology 24:87-92; Buckley, J., et al. 1994. “Epidemiological characteristics of Childhood Acute Lymphocytic Leukemia,” Leukemia 8(5):856-864. 18. Repetto, R., et al. 1996 March. Pesticides and Immune System: The Public Health Risk, World Resources Institute, Washington, DC. 19. Hardell, L., et al. 1999 Mar. “A Case-Control Study of Non-Hodgkins Lymphoma and Exposure to Pesticides,” J of the Am Cancer Soc, (85):6. p.1353. 20. Osburn, S. 2001. Do Pesticides Cause Lymphoma? Lymphoma Foundation of America, Chevy Chase, MD. 21. Cox C. 2004 Winter. “Glyphosate.” Journal Of Pesticide Reform Vol. 24 (4). 22. Rudant, J. et al. 2007. Household Exposure to Pesticides and Risk of Childhood Hematopoietic Malignancies: The ESCALE Study (SFCE). Environ Health Perspect. 115:1787–1793. 23. Canadian Partnership For Children’s Health and Environment. 2007. A Father’s Day Report - Men, Boys And Environmental Health Threats. www.healthyenvironmentforkids.ca. 24. Hernández, AF., Parrón, T. and Alarcón, R. 2011. Pesticides and asthma. Curr Opin Allergy Clin Immunol.11(2):90-6 25. Raanan R, Harley KG, Balmes JR, et al. 2015. Early-life exposure to organophosphate pesticides and pediatric respiratory symptoms in the CHAMACOS cohort. Environ Health Perspect. 123(2):179-85. 26. Liu B, Jung KH, Horton MK, et al. 2012. Prenatal exposure to pesticide ingredient piperonyl butoxide and childhood cough in an urban cohort, Environ Int. 48:156-61. 27. Salam, MT, et al. 2004. “Early Life Environmental Risk Factors for Asthma: Findings from the Children’s Health Study.” Environmental Health Perspectives 112(6): 760. 28. Boyle, C. A., et al. 1994. “Prevalence and health impact of developmental disabilities in US children.” Pediatrics 93: 399-403. 29. National Research Council. 2000. Scientific frontiers in developmental toxicology and risk assessment. Washington, DC: National Academy Press; Physicians for Social Responsibility, The National Environmental Trust, and the Learning Disabilities Association of America. 2000. Polluting our future: Chemical pollution in the U.S. that affects child development and learning. http://www.net.org/health/tri_report.pdf (accessed 6/2/05). 30. Marks AR, Harley K, Bradman A, Kogut K, Barr DB, Johnson C, et al. 2010. Organophosphate Pesticide Exposure and Attention in Young Mexican-American Children: The CHAMACOS Study. Environ Health Perspect 118:1768-1774. 31. Landrigan, P.J., L Claudio, SB Markowitz, et al. 1999. “Pesticides and in¬ner-city children: exposures, risks, and prevention.” Environmental Health Perspectives 107 (Suppl 3): 431-437. 32. Greenlee, A. et al. 2004. “Low-Dose Agrochemicals and Lawn-Care Pesticides Induce Developmental Toxicity in Murine Preimplantation Embryos,” Environmental Health Perspectives 112(6): 703-709; Cavieres, M., et al. 2002. “Developmental toxicity of a commercial herbicide mixture in mice: Effects on embryo implantation and litter size.” Environmental Health Perspectives 110:1081-1085. 33. Shelton, Geraghty, Tancredi. 2014. Neurodevelopmental Disorders and Prenatal Residential Proximity to Agricultural Pesticides: The CHARGE Study. Environmental Health Perspectives:122(10). 34. Wagner-Schuman, M, Richardson, J, Auinger, P et al. 2015. Association of pyrethroid pesticide exposure with attention-deficit/hyperactivity disorder in a nationally representative sample of U.S. children. Environmental Health. 14:44 35. Porter, W. 2004 Spring. “Do Pesticides Affect Learning and Behavior? The neuro-endocrine-immune connection,” Pesticides and You, Beyond Pesticides 21(4): 11- 15; Shettler, T., et al. 2000. “Known and suspected developmental neurotoxicants,” In Harms Way: Toxic Threats to Child Development, Greater Boston Physicians for Social Responsibility: Cambridge, MA; Mitchell, J. et al. 1989. “The Behavioral Effects of Pesticides in Male Mice,” Neurotoxicology and Teratology 11: 45-50. 36. Cox C. 2004. Journal Of Pesticide Reform Vol. 24 (4) citing: Garry, V.F. et al. 2002. “Birth defects, season of conception, and sex of children born to pesticide applicators living in the Red River Valley of Minnesota.” Environmental Health Perspectives 110 (Suppl. 3):441-449. 37. Garry, V., et al. 1996. “Pesticide appliers, biocides, and birth defects in rural Minnesota.” Environmental Health Perspectives 104(4):394-399. 38. EPA. 2004 June. 2,4-D. HED’s Human Health Risk Assessment for the Reregistration Eligibility Decision (RED). p7. 39. Centers for Disease Control and Prevention. 2003 Jan. Second National Report on Human Exposure to Environmental Chemicals. 40. Valcke, Mathieu, et al. 2004. “Characterization of exposure to pesticides used in average residential homes with children ages 3 to 7 in Quebec.” Nat Inst of Public Health, Québec. www.inspq.qc.ca/pdf/publica-tions/319-CaracterisationPesticidesEnfants.pdf (accessed 6/2/05). 41. Nishioka, M., et al. 1996. “Measuring lawn transport of lawn-applied herbicide acids from turf...” Env Science Technology, 30:3313-3320; Nishioka, M., et al. 2001. “Distribution of 2,4-D in Air and on Surfaces Inside Residences...”Environmental Health Perspectives 109(11). 42. Morgan, M, Wilson, N, and Chuang C. 2014. Exposures of 129 Preschool Children to Organochlorines, Organophosphates, Pyrethroids, and Acid Herbicides at Their Homes and Daycares in North Carolina. Int. J. Environ. Res. Public Health, 11(4), 3743-3764 43. Rudel, Ruthann, et al. 2003. “Phthalates, Alkylphenols, Pesticides, Polybrominated Diphenyl Ethers, and Other Endocrine-Disrupting Compounds in Indoor Air and Dust.” Environmental Science and Technology 37(20): 4543-4553. 44. Lu, C. et al. 2008. Dietary Intake and Its Contribution to Longitudinal Organophosphorus Pesticide Exposure in Urban/Suburban Children. Environmental Health Perspectives doi:10.1289/ehp.10912 available via http://dx.doi.org/. 45. Roberts, C. et al. 2007. Maternal Residence Near Agricultural Pesticide Applications and Autism Spectrum Disorders among Children in the California Central Valley. Environmental Health Perspectives 115(10) 46. Alarcon, WA. et al. 2005. Acute illnesses associated with pesticide exposure at school. J Am Medical Association 294(4); 455-465.
Source:
https://www.beyondpesticides.org/assets/media/documents/lawn/factsheets/Pesticide.children.dontmix.pdf
Yard Chemicals Harm Pets…


 Of those same
Of those same